Midwives have been supporting women through pregnancy and childbirth for centuries, yet so many people still misunderstand what midwifery is—and what it isn’t.
How to Know If You Have an Ovarian Cyst: A Guide for Women in Cumming, GA
Ovarian cysts are a common concern among women, yet many remain uncertain about their symptoms and when to seek medical attention.
What’s Normal “Down There” After Vaginal Birth – And What’s Not
Giving birth is a powerful, life-changing experience—and it also changes your body in ways you may not have expected. If you’ve recently delivered a baby vaginally and are wondering what’s supposed to feel different “down there” (and what might need a doctor’s attention), you’re not alone.
Top 10 Tips for Breastfeeding Twins
Breastfeeding twins presents unique challenges, but with the right strategies and support, many mothers find it to be a rewarding experience. At North Pointe OB/GYN in Cumming, GA, we understand the complexities involved and are here to offer guidance.
The Hidden Connection: How Eating Disorders Impact Menstrual Health
When it comes to women’s health, nutrition and reproductive wellness are closely intertwined. At North Pointe OB/GYN in Cumming, we regularly educate patients about the impact of diet and lifestyle on menstrual cycles.
Carrier Screening: Understanding Your Baby’s Genetic Health Before Birth
Every expecting parent wants a healthy pregnancy and a bright future for their baby. While most pregnancies progress smoothly, some genetic conditions may be passed down unknowingly. Carrier screening is a valuable tool that helps parents understand their baby’s genetic risks before birth, providing peace of mind and preparation for the future.
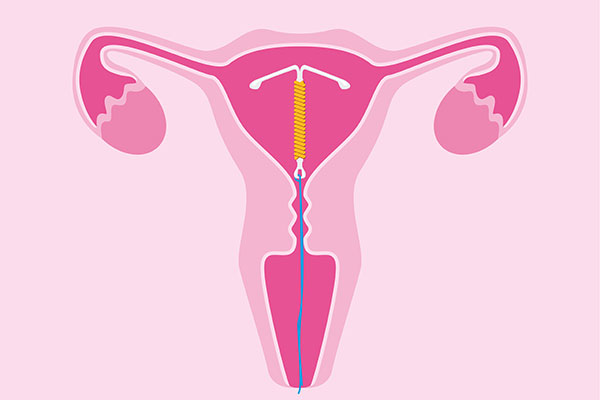
The Pros and Cons of an IUD for Birth Control: Is It Right for You?
Choosing the right birth control method is a highly personal decision, and for many women, an intrauterine device (IUD) offers a convenient and highly effective option. At North Pointe OB/GYN in Cumming, we help patients navigate their birth control choices, ensuring they find the method that best suits their lifestyle and reproductive health goals.
Period Cramps: What’s Really Happening and When to Seek Help
Menstrual cramps are a common experience for many women, but if you’ve ever wondered why they happen or why some months seem worse than others, you’re not alone. At North Pointe OB/GYN in Cumming, we’re here to help you better understand your body and manage uncomfortable period symptoms.
Pregnancy Headaches: Causes, Relief, and When to Call Your OB/GYN
Pregnancy is a time of joy and anticipation, but it also comes with its share of physical changes—some of which may bring unexpected discomfort. For many women, headaches become a common occurrence during pregnancy. While most are harmless, they can still be frustrating and sometimes signal the need for medical attention.
Do These 5 Things Before Getting Pregnant in 2025
Planning for a baby is an exciting journey, and preparing your body and mind beforehand can make all the difference in ensuring a healthy pregnancy and a happy start to parenthood. At North Pointe OB/GYN in Cumming, we’re here to support you every step of the way. As you look ahead to 2025, consider these five essential steps before getting pregnant to optimize your health…